

Exciting News from Medical by BOB!
Exciting News from Medical by BOB! Hey there! We’re thrilled to announce that Medical by BOB is launching its very own blog soon! Dive
Sign Up For Newsletter
Pediatric Medical Equipment & Devices
Smart beds to improve sleep safety for children with extra care needs.
Sensory-friendly enclosed beds designed to improve children’s sleep quality.
At-Home Care Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
Sensory-friendly enclosed beds designed to improve sleep quality.
Maternal/Postpartum Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
CGMs/Diabetes Support
Explore our comprehensive CGM comparison guide featuring Dexcom G6, Dexcom G7, FreeStyle Libre 2, and FreeStyle Libre 3, and find the right diabetes management support offered through insurance coverage.
Elder Care Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
About Us & Community
Product Knowledge
Assistance & FAQs
Pediatric Medical Equipment & Devices
Smart beds to improve sleep safety for children with extra care needs.
Sensory-friendly enclosed beds designed to improve children’s sleep quality.
At-Home Care Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
Sensory-friendly enclosed beds designed to improve sleep quality.
Maternal/Postpartum Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
CGMs/Diabetes Support
Explore our comprehensive CGM comparison guide featuring Dexcom G6, Dexcom G7, FreeStyle Libre 2, and FreeStyle Libre 3, and find the right diabetes management support offered through insurance coverage.
Elder Care Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
About Us & Community
Product Knowledge
Assistance & FAQs
Pediatric Medical Equipment & Devices
Smart beds to improve sleep safety for children with extra care needs.
Sensory-friendly enclosed beds designed to improve children’s sleep quality.
At-Home Care Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
Sensory-friendly enclosed beds designed to improve sleep quality.
Maternal/Postpartum Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
CGMs/Diabetes Support
Explore our comprehensive CGM comparison guide featuring Dexcom G6, Dexcom G7, FreeStyle Libre 2, and FreeStyle Libre 3, and find the right diabetes management support offered through insurance coverage.
Elder Care Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
About Us & Community
Product Knowledge
Assistance & FAQs
Pediatric Medical Equipment & Devices
Smart beds to improve sleep safety for children with extra care needs.
Sensory-friendly enclosed beds designed to improve children’s sleep quality.
At-Home Care Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
Sensory-friendly enclosed beds designed to improve sleep quality.
Maternal/Postpartum Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
CGMs/Diabetes Support
Explore our comprehensive CGM comparison guide featuring Dexcom G6, Dexcom G7, FreeStyle Libre 2, and FreeStyle Libre 3, and find the right diabetes management support offered through insurance coverage.
Elder Care Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
About Us & Community
Product Knowledge
Assistance & FAQs
Pediatric Medical Equipment & Devices
Smart beds to improve sleep safety for children with extra care needs.
Sensory-friendly enclosed beds designed to improve children’s sleep quality.
At-Home Care Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
Sensory-friendly enclosed beds designed to improve sleep quality.
Maternal/Postpartum Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
CGMs/Diabetes Support
Explore our comprehensive CGM comparison guide featuring Dexcom G6, Dexcom G7, FreeStyle Libre 2, and FreeStyle Libre 3, and find the right diabetes management support offered through insurance coverage.
Elder Care Medical Equipment & Devices
Non-intrusive, easy pelvic floor therapy for women’s incontinence.
About Us & Community
Product Knowledge
Assistance & FAQs
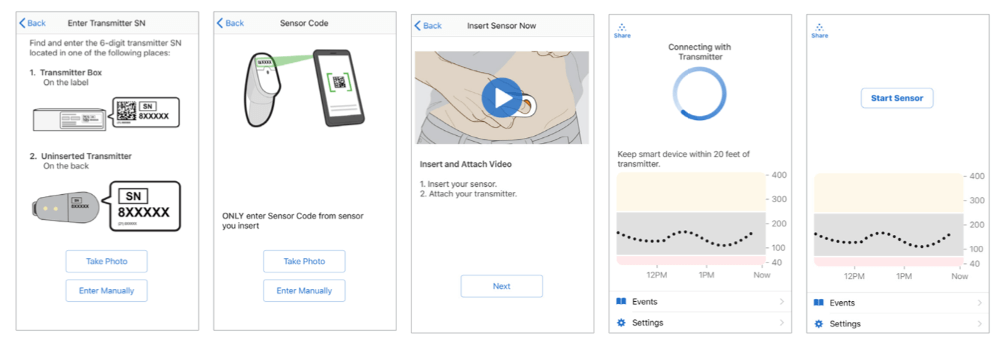
We’re proud to announce that the groundbreaking Dexcom Products are now available through the Durable Medical Equipment (DME) services at Baby’s on Broadway.
Dexcom is revolutionizing the way diabetes is managed in our community. A breakthrough in medical technology, Dexcom G6 & G7 offers accurate, real-time glucose readings, straight to your smartphone or smartwatch. With its user-friendly design, this innovative system simplifies diabetes management, helping you make confident decisions about food, activities, and overall health.
Explore our range of Dexcom products and join the fight for better diabetes control.
Select your insurance provider & select your product
We'll verify your coverage and handle all the paperwork
Sit back and wait for your product to arrive
Dexcom is proud to have teamed up with the best insulin delivery devices, health apps, and companies to advance diabetes treatment with new platforms and integrations, making treatment more customizable and convenient than ever. Dexcom Continuous Glucose Monitoring (CGM) Systems connect to more apps, insulin pumps, and technology than any other brand — so you can manage your diabetes anytime, anywhere.


Dexcom CGM helps you live your best life with connections you use every day, so you can see your glucose numbers and take better control of your diabetes.




Explore Dexcom’s innovative glucose monitoring systems that are revolutionizing diabetes management. Designed with state-of-the-art technology, these products provide real-time, accurate glucose readings, paving the way for a healthier future for those living with diabetes. Experience the difference with Dexcom’s trailblazing solutions.
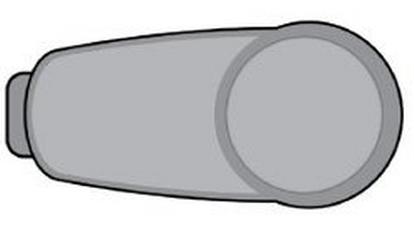
Dexcom G7, the simple CGM system, delivers real-time glucose numbers to your smartphone* or smart watch‡—no fingersticks required.† Effortlessly see your glucose levels and where they’re headed, so you can make smarter decisions about food and activity in the moment to take better control of your diabetes.
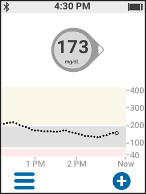
The Dexcom G6 Continuous Glucose Monitoring (CGM) system sends your glucose numbers to a smart device* every 5 minutes without fingersticks† or scanning. Trend arrows show where your numbers are heading and how fast, making it easier to make better management decisions.


Dexcom G6 and Dexcom G7 let you share your glucose levels with up to 10 people who use the separate Dexcom Follow app, giving you an added layer of support. Followers can see your glucose numbers remotely from their smart devices.




You should order Dexcom G6. As soon as your connected pump integrates with Dexcom G7, you will be able to switch to Dexcom G7.
Product | Advantages | Professional Tips |
Smith and Nephew IV Prep | – Waterproof, breathable barrier film – Also contains alcohol for antiseptic properties | – Comes in wipes – Let dry completely on skin – Not marketed as having tackifying properties, but may see mild enhancement to adhesiona |
Bard® Protective Barrier Film | – Waterproof, breathable barrier film | – Comes in wipes or spray – Does not include antiseptic |
SurePrep™ (Medline) | – Vapor permeable barrier film – Includes antiseptic | – Comes in wipes – Can be used on damaged skin as protection |
Smith and Nephew Skin prep/no-sting skin prep | – Waterproof, breathable barrier film – Popular choice due to moderate protection and moderate adhesive properties combineda | – Comes in wipes or spray – Skin prep indicated for intact skin, no-sting skin prep indicated for intact or damaged skin – Does not include antiseptic |
Cavilon™ No Sting Barrier (3M™) | – Waterproof, breathable barrier film | – Comes in wipes or spray – Does not include antiseptic |
AllKare® Protective Barrier Wipe | – Waterproof, breathable barrier film | – Comes in wipes – Does not include antiseptic |
Product | Advantage | Professional Tips |
Hydrocolloid dressings: – DuoDERM® – Toughpads – (Dynarex) Dynaderm™ – BAND-AID® Brand HYDRO SEAL® | – Hydrocolloid provides thick protection – Waterproof – Some brands have ‘‘extra thin’’ version – Some latex free | – Offers stronger barrier protection than an adhesive patch, such as IV 3000 or Tegaderm |
IV3000 (Smith&Nephew) | – Transparent, thin film, precut patch – May be less irritating than sensor adhesives | – May also be used as an adhesive enhancer when placed over sensor tape – More prone to peel with water, sweating, humiditya – Many patients report less skin reaction with IV3000 compared with Tegaderma |
Tegaderm or Tegaderm HP | – Transparent, thin film, precut patch | – HP stands for ‘‘Holding Power’’ and may adhere more strongly than standard Tegaderm – May also be used as an adhesive enhancer when placed over sensor tape – More prone to peel with water, sweating, humiditya |
Opsite/Flexifit (Smith&Nephew) | – Roll of thin transparent film can be cut to size | – May also be used as an adhesive enhancer when placed over sensor tape |
COMPEED® Plasters | – Absorbs moisture on skin, possibly aiding adhesion | – Original intention as blister cushion – Adheres better after warming to skin temperature in hands before applicationa |
Product | Advantages | Professional Tips |
Fluticasone propionate nasal spray (generic). Common examples: – Flonase® Allergy Relief – Flonase® Children’s Allergy Relief – Clarispray® Nasal Allergy Spray | – May prevent mild, moderate, and severe skin reactions due to CGM adhesive | – Apply 2 puffs to sensor site. Wait 2 minutes for spray to dry. Insert sensor as usual. |
Product | Description |
Uni-solve Adhesive Remover (Smith&Nephew) | – Comes in wipes or liquid |
AllKare Adhesive Removal Wipe (ConvaTec Inc) | – Comes in wipes |
Tac Away Adhesive Removal Wipes (Torbot) | – Comes in wipes – Reciprocal product to Skin Tac |
Detachol Adhesive Remover (Eloquest) | – Latex free, alcohol free – Comes in single use vials or liquid – Reciprocal product to Mastisol |
Household oilsa: – Baby oil, coconut oil or olive oil | – Least specialized and least expensive option |
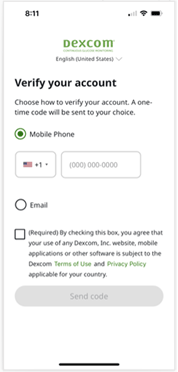 | To set up and verify your account using your mobile number, simply:
|
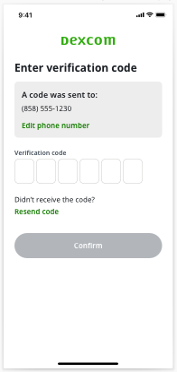 | When you get the code:
|
Troubleshooting | |
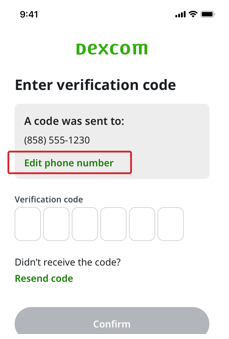 | I entered my mobile number incorrectly.
|
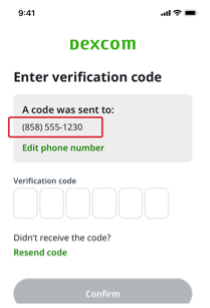 | I didn’t get a code.
|
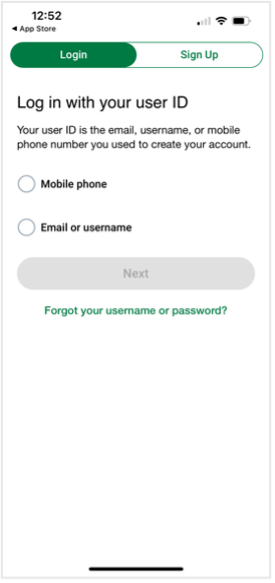 | On the log in screen:
On the next screen:
On the log in screen:
On the next screen:
|
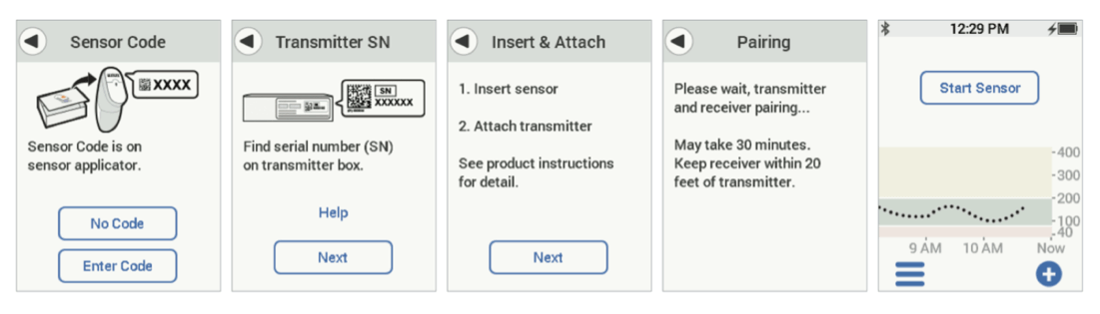
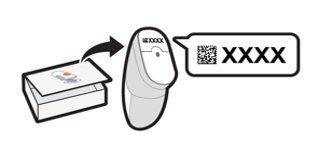
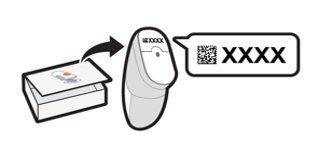
Yes, you’ll need to put in the sensor code from the sensor each time you start a new one. The sensor code is found on the bottom of the applicator on the adhesive strip.
 Dexcom G6 Touchscreen Receiver | 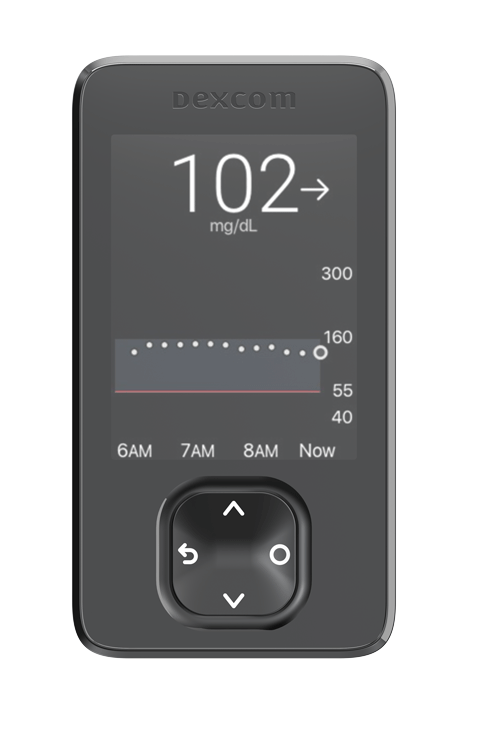 NEW Dexcom G6/G7 Receiver |
The Urgent Low Soon alert can warn users in advance (within 20 minutes) of a severe hypoglycemic event (55 mg/dL), which helps give them time to take appropriate action before an event occurs.
New features with Dexcom G7 | Dexcom G6 features included with Dexcom G7 |
|
|
More insight than using a meter alone
Improved glycemic control
Fast, proactive response
Fewer fingersticks
Fewer worries
As with all previous generations of Dexcom CGM, Dexcom G6 will eventually be discontinued. Until then, G6 will still be available, and we are working closely with all our partners to transition users from G6 to G7 as smoothly and as efficiently as possible.

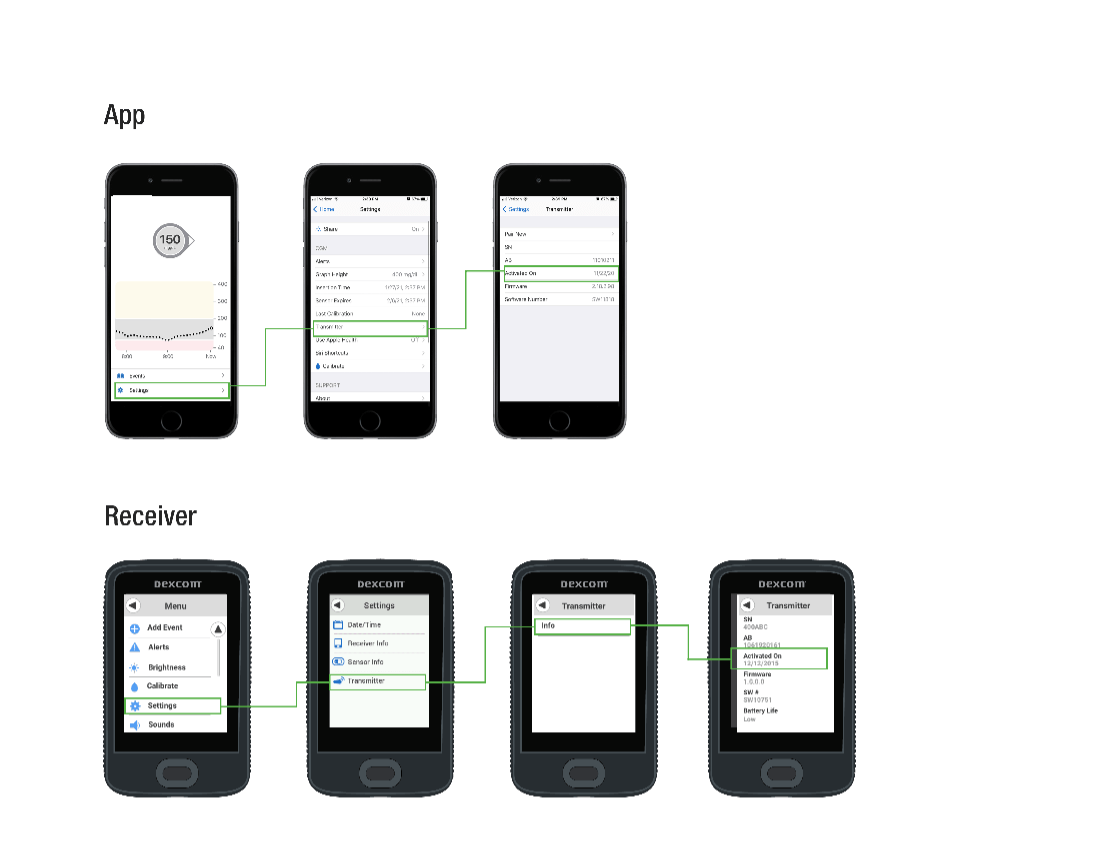
Use Settings to customize data display and sharing. Changes only apply to Dexcom Clarity and do not change any settings on your Dexcom CGM system.
All data uploaded to Dexcom Clarity will remain accessible as long as the product is available for use. When logging in to Dexcom Clarity for the first time, there will be limited data depending on when the account was created. Going forward, data will continue to build as it is uploaded to Dexcom Clarity.
Under the Devices section of Dexcom Clarity’s Overview report you will find the alert settings and last uploads for the CGM systems used. Device settings are for your reference and are separate from Dexcom Clarity settings. This information can only be found on the web version of Dexcom Clarity at clarity.dexcom.com
Yes, you can generate PDFs for all Dexcom Clarity reports to view, save, print, or email.
See how metrics are calculated in Dexcom Clarity in the Glossary.
If you enter events such as carbs or exercise on both your receiver and your smart device, then both the receiver and the smart device must be uploaded to Dexcom Clarity to show complete data and accurate statistics.
Product | Advantages | Professional tips |
No-Sting skin Prep (Smith&Nephew)  | -Provides barrier protection | – Comes in wipes or liquid – Not as strong as Skin Tac or Mastisol |
Skin Tactm(Torbot) 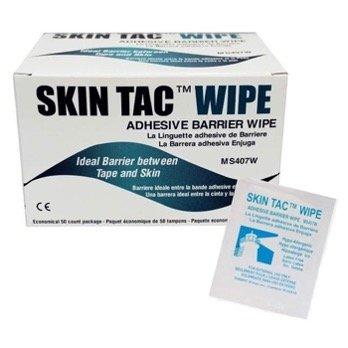 | – Provides barrier protection – Higher adhesive properties than Skin Prep – Latex-free, hypoallergenic, nonrubber adhesive | – Comes in wipes or liquid – Consider use of reciprocal removal product – Tac Away |
Mastisol® Liquid Adhesive (Eloquest)  | – Higher adhesive properties than Skin Prep or Skin Tac | – Comes in liquid, swabs, or single use vials – Consider use of reciprocal removal product -Detachol |
Product | Advantages | Professional tips |
IV3000 (Smith&Nephew) 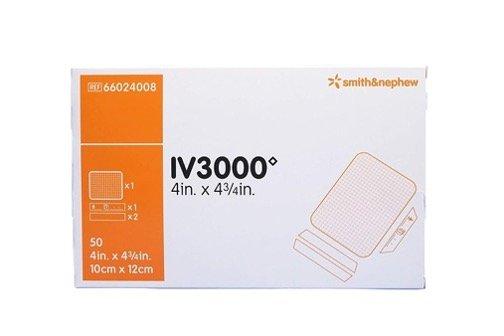 | – Thin transparent film – May cause fewer reactions than Tegaderm | – May also be used as a barrier when placed under sensor tape – Not breathable, may peel with sweating or if water gets under |
Tegaderm HP (HP stands for ‘‘Holding Power’’)  | – Thin transparent film – May adhere more strongly than standard Tegaderm | – Not breathable, may peel with sweating or if water gets under |
Hypafix®  | – Thicker, fabric-like adhesive than transparent films – Can be cut to size – Excellent adhesion even when wet | – Excellent staying power and thickness – May cause less trauma to skin upon removal2 |
Opsite™/Opsite Flexifit™ (Smith&Nephew)  | – Breathable, transparent film with moderate permeability | – Can come as precut patches or in a roll |
Blenderm™ (3M)  | – Clear plastic hypoallergenic tape | – Comes in a tape roll, best used as a supplement to counteract peeling patch |
Transpore™ Surgical Tape  | – Clear, porous, plastic hypoallergenic tape | – Comes in a tape roll, best used as a supplement to counteract peeling patch |
Kinesiology tape:
 | – Comes in a roll for custom cutting – Gentle on skin with mild stretch | – Similar material to RockaDex and GrifGrips |
Cloth-like patches:
 | – Precut for CGM – Flexible and breathable – Excellent adhesion even when wet – Bright colors and shapes | – Similar materials to kinesiology tapes and may be stretched or cut to fit a variety of devices and body shapes |
Nonadhesive wraps:
 | – If you are unable to tolerate additional adhesive, wraps may help keep your sensor in place | – Wrap loosely, do not compress skin with elastic wraps – Remove during nighttime to avoid tissue compression – Consider for short-term use—during sports, activity, etc. |
Yes, Dexcom G7 can be worn during pregnancy for all types of diabetes (type 1, type 2, or gestational).
Dexcom G7 is factory calibrated. Unlike G6 sensors, the G7 sensors are pre-programmed with the factory calibration setting so you don’t need to enter a sensor code. However, you will still need to enter the 4-digit pairing code provided on the body of each new G7 applicator to pair a sensor to your compatible smart device* or receiver.


*Compatible smart devices sold separately. To view a list of compatible smart devices, visit dexcom.com/compatibility
Dexcom G7 is for patients two years and older with any type of diabetes including type 1, type 2, or gestational diabetes.
At security checkpoints
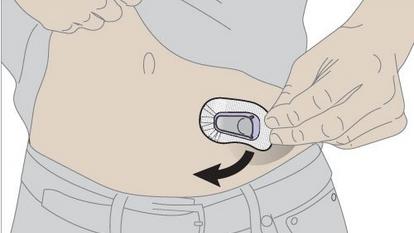
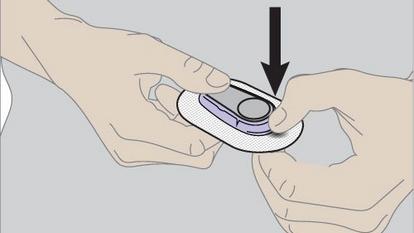
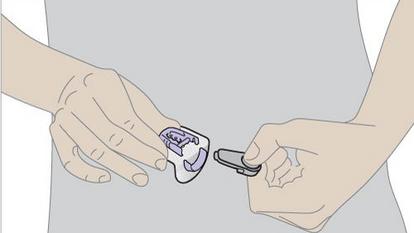
How to insert your Dexcom G7 sensor
How to apply your overpatch


If you were prescribed G7 and you need to switch back to Dexcom G6, reach out to your doctor and obtain a new prescription for Dexcom G6. Healthcare Providers should continue to prescribe G6 for patients seeking (or using) automated insulin delivery systems until G7 is compatible with their preferred AID system of choice.
*Compatible smart devices sold separately. To view a list of compatible smart devices, visit dexcom.com/compatibility
Focus Mode
App Pause
Battery Saver Mode
Adaptive Battery
Battery Optimizing
Optimized Battery Charging
Device Bluetooth
Location
Nearby Device Permission
Notifications Permission
Background Restrictions
Do Not Disturb (DND) Permission




Screen Time
Do Not Disturb
Low Power Mode
Optimized Battery Charging
Device Bluetooth
Notifications Permission
Critical Alerts


Yes, Dexcom G7 works with Dexcom Clarity. Users who used Dexcom Clarity with Dexcom G6 do not need to register again. The G7 app also conveniently integrates a Clarity data summary (called the Clarity card) into the home screen of the G7 app for quick and easy insights. Learn more about Dexcom Clarity here.
iPhone




Android


Dexcom G7 sensors may be inserted on the back of the upper arm (indicated for users ages 2 years and older) or the upper buttocks (ages 2-6 years old). Our research shows that back of the upper arm wear results in optimal performance*. Sensor placement is important, and you should change your insertion site with each sensor. Using the same site too often might not allow the skin to heal, causing scarring or skin irritation. Be sure to use the overpatch included with your G7 sensor; this will help ensure your sensor will remain in place for the duration of the wear session.
Applying your sensor


Applying the overpatch




Dexcom Share is a feature within the Dexcom G7 app that allows for remote monitoring. One person (the Sharer) may share their CGM data with up to 10 designated individuals (the Followers).
To set up the Share feature in the Dexcom G7 app, go to Connections > Share and follow the onscreen instructions. Always make treatment decisions using the primary Dexcom G7 app, not the Dexcom Follow app.
The Dexcom G7 sensor is indicated to be worn for up to 10 days, with a 12-hour grace period at the end.
New features with Dexcom G7 | Dexcom G6 features included with Dexcom G7 |
|
|








Bothered by High Alerts after you eat, even though you took insulin? Talk to your healthcare provider about using the Delay 1st High Alert feature in Profile > Alerts > High. Use it to avoid getting an alert until your glucose has been high for a few hours, or long enough for the insulin to have worked.


Insulin and food both take time to work. Avoid getting repeated alerts while you wait. To do so, go into the alert settings and turn off the Snooze feature.
The trend arrow tells you the speed and direction of your glucose level. There are times that the Dexcom G7 sensor may be temporarily unable to accurately measure this and will not show trend arrow on your display device. When this happens, make sure to use your blood glucose meter to make diabetes treatment decisions.
You can see the events you’ve tracked on your display device. On the receiver, navigate to the Event Log, and you’ll see a list of the last 15 events you logged.


After you upload your receiver data to the Dexcom Clarity app or website, your events will be in your Clarity reports. Go to the Dexcom Clarity appendix for more information.


Smartphone App:


iOS
Android
G7 Receiver:








*Please note: Your sensor readings come from different fluids than your BG meter values, so the two usually won’t match. Neither number is as accurate as the lab test your healthcare provider performs. For more information on accuracy and calibrating your Dexcom G7, refer to the Accuracy and Calibration section of the Dexcom G7 User Guide.


*Please note: Your sensor readings come from different fluids than your BG meter values, so the two usually won’t match. Neither number is as accurate as the lab test your healthcare provider performs. For more information on accuracy and calibrating your Dexcom G7, refer to the Accuracy and Calibration section of the Dexcom G7 User Guide.
Dexcom is working closely with our insulin pump partners to integrate Dexcom G7 into current and future automated insulin delivery (AID) systems as quickly as possible. Please reach out to the pump company for the most current launch timelines.
Dexcom G7 gives you a graph that shows where your glucose has been. Event logging can help you understand why your glucose changed. For example, what happened to your glucose level when you took a walk after breakfast? Discuss your reflections with your healthcare provider to learn more ways to manage your blood glucose.
Children ages 2-6 years old can wear the Dexcom G7 sensor on the upper buttocks. To support the accuracy and effectiveness data submitted for Dexcom G7, we enrolled subjects ages 2-6 years for upper buttocks wear location. The subjects 7 years and older wore only on the arm in this study.
Site preparation
Patch care




Yes, Dexcom G7 Continuous Glucose Monitoring (CGM) system is indicated for pediatric patients two years and older with any type of diabetes.
The G7 sensors are indicated for use on back of upper arms because, during testing, users who wore it there had optimal system performance.
The “Bluetooth is off” alert means this function is turned off. It will either show as App Bluetooth is off or Phone Bluetooth is off. Bluetooth must be on to get glucose information on your display device. * Refer to your smart device guide to turn on your Bluetooth.
See Our Android and iPhone Settings FAQs
To share glucose data with Apple Health:
Dexcom recommends that users dispose of used Dexcom G7 applicators following local guidelines for blood-containing components.
No. Dexcom recommends using either Dexcom G6 or Dexcom G7, but not both simultaneously.


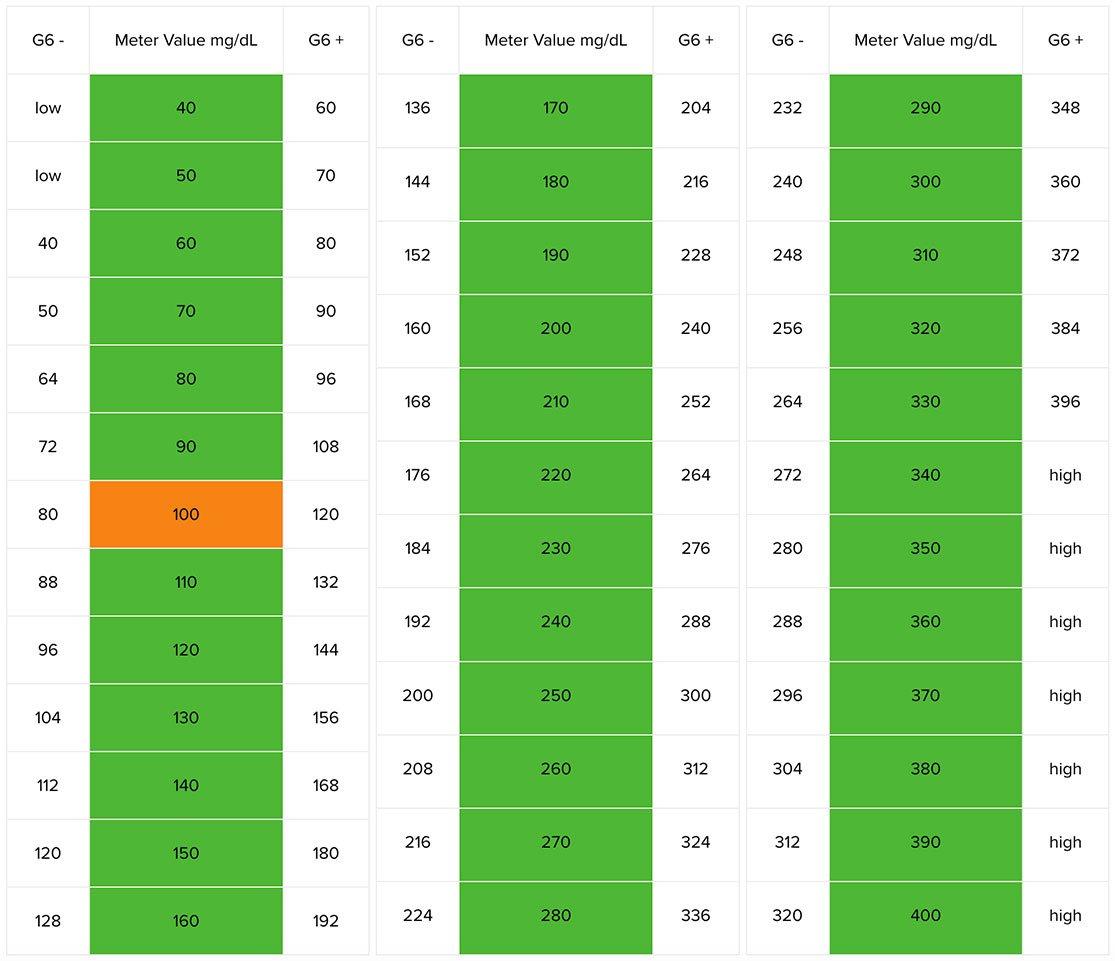
Calibrating vs. Comparing
Comparing


Calibration Tips:








See Our Dexcom G7 Videos – How to Insert the Sensor & Applying the Overpatch
You can turn off most alerts in their settings. The alerts you can’t turn off in their settings – Urgent Low and technical alerts (like Sensor Fail) – can be set to vibrate using Quiet Modes in the app or Alert Sounds on the receiver.









Dexcom G6 is designed to not impact your travel. You can go through metal detectors, be hand-wanded, and even keep your receiver on during your flight.
Dexcom designed the Dexcom G6 CGM System sensor auto-applicator for easier, more consistent sensor insertions. We recommend viewing the Dexcom G6 Videos for a helpful demonstration of the sensor insertion and transmitter attachment process. The video is available in both English and Spanish.
The Dexcom G6 auto applicator was designed for easier, more consistent sensor insertions. According to a survey of Dexcom G6 users, 84% reported that the initial sensor insertion was painless and 100% reported that the applicator was easy to use.
For study details, please reference the Dexcom G6 user guide.
Dexcom G6 sensor replacement frequency: A single Dexcom G6 sensor can be worn up to 10 days. For tips on keeping your sensor on for the full 10-day wear, please reference the sensor adhesive tips.
To learn more about how to change your Dexcom G6 sensor after 10 days of wear, see our Dexcom G6 videos.
How to remove your Dexcom G6 sensor and transmitter:
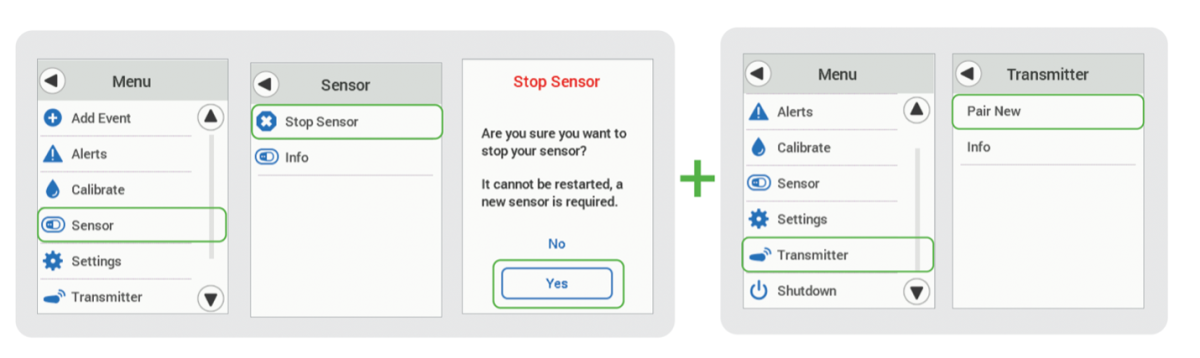
Start a new Dexcom G6 sensor session
Yes, Dexcom G6 is compatible with the Dexcom Clarity software. Patients will not need to register again, nor download a new Dexcom Clarity app, if they have an existing account. If you are already sharing your glucose data with your clinic, the clinic will not need to reconnect. For more information on Dexcom Clarity, please visit clarity.dexcom.com.
Without your sensor code, you’ll need to calibrate twice after your 2-hour sensor warmup is complete, a third time 12 hours later, a fourth time 12 hours after that, and then once every 24 hours.

The Urgent Low Soon alert is designed to notify you when your Dexcom G6 reading is predicted to reach 55 mg/dL within 20 minutes. The Fall Rate is designed to notify you when your glucose level is falling 2 or 3 mg/dL each minute. For more information, please visit page 144 in the Dexcom G6 CGM User Guide.
Yes, Dexcom G6 is indicated for children as young as 2 years old.
If you’re seeing this message, it means that your phone isn’t compatible with the Dexcom G6 app. As a result, you can’t install the app at this time.
You must use a phone listed at www.dexcom.com/compatibility to install the app. These are Android phones that have passed our compatibility testing.
If you can see the introducer needle sticking out, please be careful that you do not poke yourself and make sure to use proper disposal methods for sharps. Make sure to only remove the safety latch after you have applied the sensor and are ready to push the button on the applicator to avoid accidental deployments. Please contact Dexcom’s Global Technical Support for a replacement sensor at 1-844-607-8398.


No. Dexcom G6 sensors are designed to last for a maximum of 10 days, after which time the Dexcom G6 will require the insertion of a new sensor.

Dexcom is working closely with our insulin pump partners to integrate Dexcom G7 into current and future automated insulin delivery (AID) systems as quickly as possible. Please reach out to the pump company for the most current launch timelines.
Dexcom G6: Auto insertion video
Dexcom G6: Setting up Dexcom Share and Follow



Choose the option that works best for you:
Use the training materials in your box to self-start, watch the online tutorials and videos, call your Healthcare Provider for training options, or call Dexcom CARE. The Dexcom CARE team of trainers and certified diabetes educators are here to help you get started with your new Dexcom CGM system.
Call 888-738-3646 to reach Dexcom CARE for live, interactive support.
Transmitter pairing failed to Omnipod® 5 ONLY (Dexcom G6 app able to pair to transmitter) |
|
Transmitter loss of connection to Omnipod® 5 ONLY (Dexcom G6 app functioning normally) |
|
Receiving an error message related to the Omnipod® 5 Pod or Omnipod® 5 App (in dedicated Controller or compatible smartphone) |
|
Physical issues with your Omnipod® 5 insulin delivery system |
|
Connecting the Dexcom G6 transmitter with Omnipod® 5 |
|
Unable to progress past the warm-up part of your sensor session |
|
Physical issues with your sensor and/or transmitter. |
|
Receiving an error message related to your transmitter lifespan |
|
Sensor replacement is independent of Omnipod® 5 replacement |
|
Sensor session doesn’t last the full 10 days |
|
Sensor doesn’t appear to be accurate |
|
Issues calibrating your Dexcom G6 CGM System |
|
We recommend continuing to use your connected system with Dexcom G6. You will be able to switch to Dexcom G7 as soon as the compatibility with our partner’s product is available and your pump system is updated (if needed).
Transmitter pairing failed to iLet ONLY (Dexcom G6 app able to pair to transmitter) | • If your Dexcom transmitter is failing to connect to the iLet, but is able to connect to the Dexcom G6 app, please contact Beta Bionics for troubleshooting at 855-745-3800. • If your Dexcom transmitter is failing to pair to both the Dexcom app and the iLet, please contact Dexcom for support at 844-607-8398. |
Transmitter loss of connection to iLet ONLY (Dexcom G6 app functioning normally) | • If you have lost connection (signal loss) between your Dexcom G6 transmitter and the iLet after initial pairing, but your Dexcom G6 app is functioning normally, please contact Beta Bionics for troubleshooting at 855-745-3800. • If your Dexcom G6 transmitter is no longer communicating to either the iLet or the G6 app, please contact Dexcom for support at 844-607-8398. |
Receiving an error message related to the iLet | • If you receive an error message related to the iLet, call Beta Bionics Customer Care at 855-745-3800. |
Unable to upload iLet pump data to Dexcom Clarity | • Pump settings and data cannot be viewed in Dexcom Clarity. That data is only available from the Beta Bionics patient/HCP portal. • The Dexcom G6 app can be used to upload your CGM data into Dexcom Clarity, where you and your healthcare professional can review it. |
Physical issues with your iLet insulin infusion set | • If you are experiencing a physical issue with your iLet infusion set such as those involving adhesion, bleeding, bruising, skin irritation, discomfort or pain at insertion site, please contact Beta Bionics for assistance troubleshooting your issue at 855-745-3800. |
Connecting the Dexcom G6 transmitter with the iLet | • The iLet connects directly to the Dexcom G6 transmitter; use of a Dexcom medical receiver isn’t supported for this automated insulin delivery system. |
Unable to progress past the warm-up part of your sensor session | • If your sensor fails during the 2-hour warm-up period, please refer to the FAQ. • If you continue to experience issues progressing beyond the initial warm-up session, please submit a Product Support Request for a replacement sensor. |
Physical issues with your sensor and/or transmitter | • Some examples of physical issues include sensor deployment difficulties, patch adhesion issues, difficulties inserting the sensor or transmitter, and discomfort during use. • See the FAQ for patch adhesion tips. • If you are experiencing a physical issue with your Dexcom G6 CGM System, please fill out a Product Support Request. |
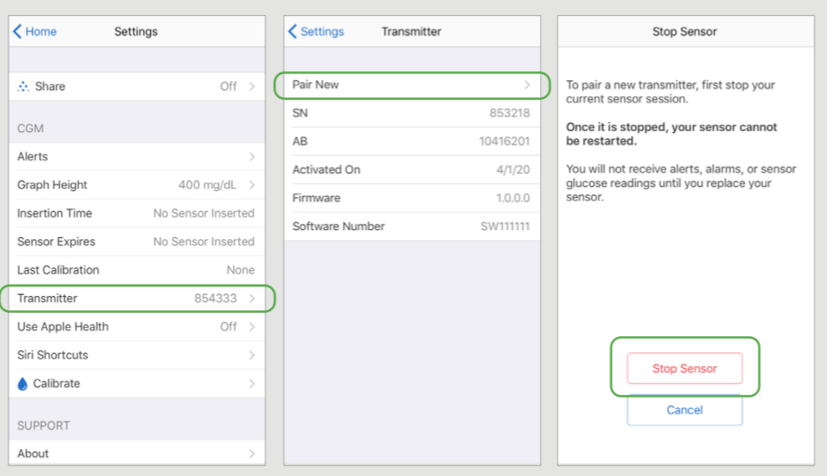
Receiving an error message related to your transmitter lifespan | • The transmitter battery lasts for 3 months after initial activation. Starting 3 weeks before the battery expires, the warnings count down the transmitter battery life until it only has 10 days – one sensor session – left. • If the transmitter battery has less than 10 days remaining, you won’t be able to start a new session and the G6 app will show “Pair New Transmitter” instead. Dexcom recommends that you have your next transmitter on hand within 3 months of starting your previous transmitter. • If you continue to experience issues with your transmitter battery, please submit a Product Support Request, or contact Dexcom Global Tech Support at 844-607-8398. |
Sensor replacement is independent of infusion set replacement | • While infusion sets are replaced every 2 to 3 days, Dexcom G6 sensors last for 10 days. You do not have to replace your sensor until your sensor session has ended. |
Sensor session doesn’t last the full 10 days | If your sensor session ended prematurely, please refer to the FAQ. You may request a replacement sensor by filling out a Product Support Request or contacting Dexcom Global Tech Support at 844-607-8398. |
Sensor doesn’t appear to be accurate | • This FAQ may also be helpful: Is my Dexcom sensor accurate? • If your sensor readings do not match symptoms or expectations, use a blood glucose meter and fingersticks to determine your glucose levels. |
Issues calibrating your Dexcom G6 CGM System | • If you entered the sensor code during set up, there’s no need to calibrate. Calibration is at the discretion of the user, but the system doesn’t require it. • If you don’t enter a sensor code, you will be prompted to manually calibrate your system using values obtained from a blood glucose meter and fingersticks. This is true for both the iLet and the G6 app. • If the calibration value from a blood glucose meter isn’t accepted by the iLet, please contact Beta Bionics Customer Care at 855-745-3800. • If the calibration value isn’t accepted by the Dexcom G6 app, please contact Dexcom Global Tech Support at 844-607-8398. • If you continue to have problems with calibrating your Dexcom G6, please submit a Product Support Request or contact Dexcom Global Tech Support at 844-607-8398. |
See the Dexcom Answers: Accuracy Video
Find and choose Dexcom G6
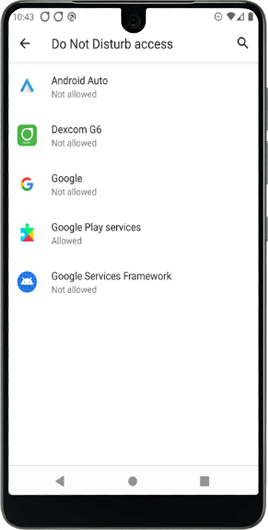
Toggle Allow Do Not Disturb to on
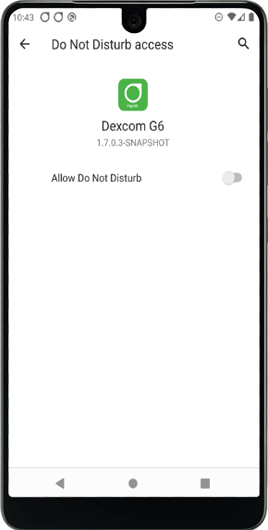
When prompted, tap Allow
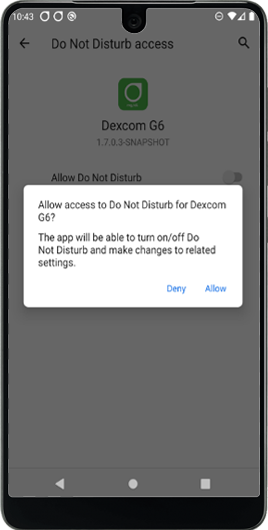
The Blue toggle indicates the Do Not Disturb Permission / Access is on.
Return to the G6 app
The Dexcom G6 CGM System’s transmitters are water resistant. The G6 Sensor Pod is water resistant when the transmitter is installed properly. The receiver is not water resistant or waterproof, and can be damaged if moisture gets inside it. Water can also severely limit communication range with the G6, so you never want to prevent communication between the transmitter and display devices. This could cause the receiver to become damaged and a patient to miss a severe low or high blood glucose event or make a treatment decision that can result in injury. There is more information available in the Dexcom G6 CGM System User Guide.




If you are receiving a Sensor Failed Alert on your Dexcom G6 and your inserted sensor will no longer give CGM values, please remove the failed sensor. Insert a new sensor and contact Tech Support (available 24/7) at dexcom.com/tech-support or call 1-888-738-3646.


Exciting News from Medical by BOB! Hey there! We’re thrilled to announce that Medical by BOB is launching its very own blog soon! Dive
*Reviews are screened and pre-approved for verified purchases only












Your Order
About BOB
Help + Info
Search
Contact Us
Request A Catalog
Privacy Policy
Terms & Conditions
Refund Policy
See All Help Topics
Your Order
About BOB
Help + Info
Search
Contact Us
Request A Catalog
Privacy Policy
Terms & Conditions
Refund Policy
See All Help Topics
Your Order
About BOB
Help + Info
Search
Contact Us
Request A Catalog
Privacy Policy
Terms & Conditions
Refund Policy
See All Help Topics
Sign up for Newsletter!
Sign Up For Newsletters and receive Free Express Shipping on your first order! Plus, you’ll receive early access to New Arrivals, Sales, Events + more
sales@babysonbroadway.com
sales@babysonbroadway.com
Copyright © 2023 Baby's On Broadway, all rights reserved.
Copyright © 2023 Baby's On Broadway, all rights reserved.